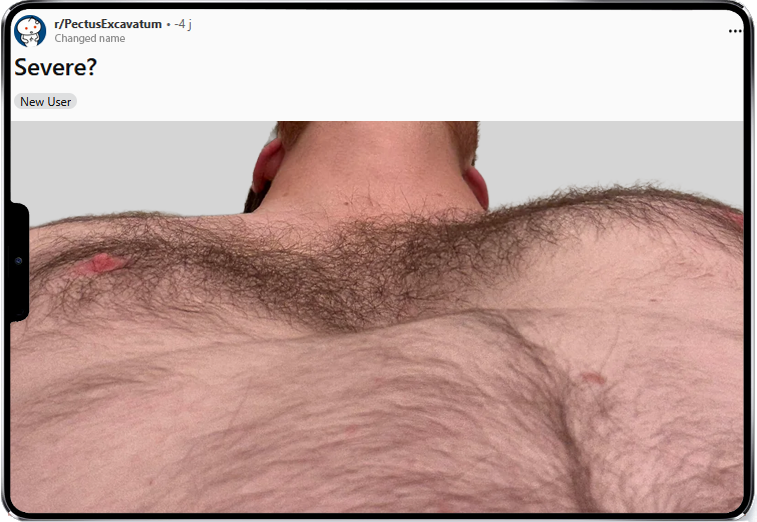
Just a few minutes on a forum like Reddit (an American community website for discussion and social news) or in the comments of a TikTok video (a Chinese mobile app for sharing short creative videos) are enough to notice it: hundreds of people post photos of their chest with a simple, anxious question: “Is my pectus serious?”.
Behind this seemingly naïve question actually lie complex concerns:
- “Is having a dip in my chest dangerous for my health?”
- “Is it normal to feel ashamed of my chest?”
- “Can I, or should I, have surgery?”
A recurring theme on social media
Anxiety visible through posts
The question “Is it serious?” comes up often because it reflects a need for validation. People who discover their chest wall deformity want to know whether it deserves attention or treatment. In an age where images dominate, this often involves posting photos on forums like Reddit (in subreddits such as r/pectusexcavatum), or via specialized TikTok videos and hashtags.
Rating your pectus
Another frequent behavior on social media is wanting to “rate” one’s sunken chest. This need for evaluation is very common:
- it’s a way of putting words on a vague feeling,
- it can be reassuring or, on the contrary, increase anxiety,
- you want to know whether you are “within the norm” or if you should do something about it.

But this trend can be misleading. A funnel chest can look “mild” on the outside and be experienced as very distressing, or the opposite. Moreover, comparing yourself to others often creates more guilt than solutions.
The Haller index: useful but incomplete
Just like rating how sunken your sternum looks, sharing your Haller index is very common online.
Some doctors use the Haller index (a calculation performed on a CT scan slice, based on the ratio of the maximum chest width to the minimum distance between the sternum and the spine at the deepest point of the depression) to assess how deep the hole in the chest is. The higher the index, the more marked the indentation is in theory.
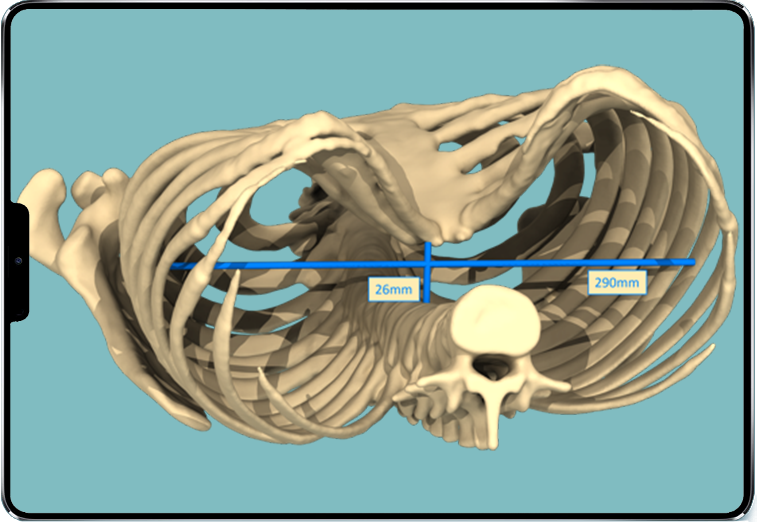
But again, caution: a high index does not necessarily mean symptoms, and the opposite is also true. This tool is one morphologic indicator among others and cannot, on its own, determine whether your chest indentation is “severe”.
Aesthetic, medical, psychological severity: three very different realities
Aesthetic severity: what is “mild” for one person can be unbearable for another
Some people live very well with a marked sunken chest, while others, with a more moderate shape, may feel:
- ashamed to undress,
- deep body dissatisfaction,
- a refusal of any social exposure (beach, sports, etc.).
Aesthetic severity deserves to be taken seriously, because it often determines quality of life on a daily basis. This is recognized by all surgeons, regardless of the technique they use.
Psychological severity: invisible… but sometimes the heaviest to bear
For many patients, the sunken sternum becomes a mental focal point. It affects:
- self-confidence,
- body image,
- romantic and sexual life.
Sometimes, the pain patients describe is linked to a consultation bias, as explained by Prof. Laurent Brouchet, Head of Thoracic Surgery at Toulouse University Hospital:
“I tend to take an observational approach and, in general, when we investigate a patient with pectus, they do not have any particular cardio-respiratory disorders. There may be a difficult psychological cardio-respiratory experience, which is often the way for children to dare to ask their parents to bring them to a consultation, and it is often a psychological defence mechanism. This can translate into pain or shortness of breath.”
He adds: “Cardiac compressions are described in the literature, but they are relatively rare and, since I’ve been practising, I’ve seen one. True cardiac compression is rare in general and is explored by the cardiology department with MRI. It remains an exceptional event. From my experience, it was 1 in 400 or 500 cases.”
Here again, we are not necessarily talking about danger for physical health, but about a real impact on mental comfort.
Medical severity: when is there a real impact on health?
There are extreme cases in which proven cardio-vascular or respiratory disorders from childhood (cardiac and/or respiratory failure) can lead to consideration of an invasive, orthopaedic correction of the chest wall.
“Pectus does not represent any danger, there is no life-threatening risk. In rare cases there may be cardio-respiratory consequences, but this is very anecdotal. The main impact is on patients’ quality of life, on the aesthetic and psychological level.”
Do you have to wait for it to be “serious” before doing something?
Apart from extreme cases with cardio-respiratory disorders, there are no “serious cases” of sunken chest in the sense of a vital emergency. And this may be the most important message. There are suitable solutions for each situation.
- In younger patients: the vacuum bell, an external suction cup, can sometimes remodel the chest wall if used early, regularly, and under medical supervision.
- In cases of functional impairment proven by a full medical work-up: sternochondroplasty (Ravitch procedure), a major orthopaedic surgery, may be considered.
- In cases of purely aesthetic or psychological discomfort, but without medical symptoms: placing a custom 3D implant, a much lighter option, can restore the appearance of the chest in a single surgery, without osteotomy or immobilisation.
The fact that it is not “serious” or “dangerous” does not mean that pectus excavatum surgery is not legitimate. Feeling bad in your body is not a weakness; it is a reality that deserves to be heard.
So how do you know whether your sunken chest “deserves” surgery? The answer is: as soon as there is discomfort, whatever its nature.
Conclusion: the real issue is not listening to how you feel
The severity of a funnel chest is not measured only by how deep the indentation is, nor by a number on a scan. It is measured by its real impact on your life — social or sporting — on your confidence and, ultimately, on your well-being.
If you are asking yourself “Is my pectus serious?”, it may already mean that it is bothering you in one way or another. And that discomfort deserves to be listened to.
Do not wait for a doctor to tell you it is serious before allowing yourself to talk about it.
Make an appointment. Ask your questions. Express how you feel.
This is the first step towards a solution tailored to your situation.



